RESIDENCY PREP
The Cross-Cover Guide is a practical, educational resource designed to support physicians during routine and urgent cross-cover issues that arise in hospitalized non-pregnant adults on medicine services.
CLICK HERE TO download the Cross-Cover Guide for free!
The Cross-Cover Guide is a practical, educational resource designed to support physicians during routine and urgent cross-cover issues that arise in hospitalized non-pregnant adults on medicine services. This guide is intended for educational purposes only and does not replace clinical judgment.
CLICK HERE to give feedback on content, organization, or kudos! We are always looking to update and improve!
Acute Clinical Emergencies
APPROACH TO RAPID RESPONSES (RRT)
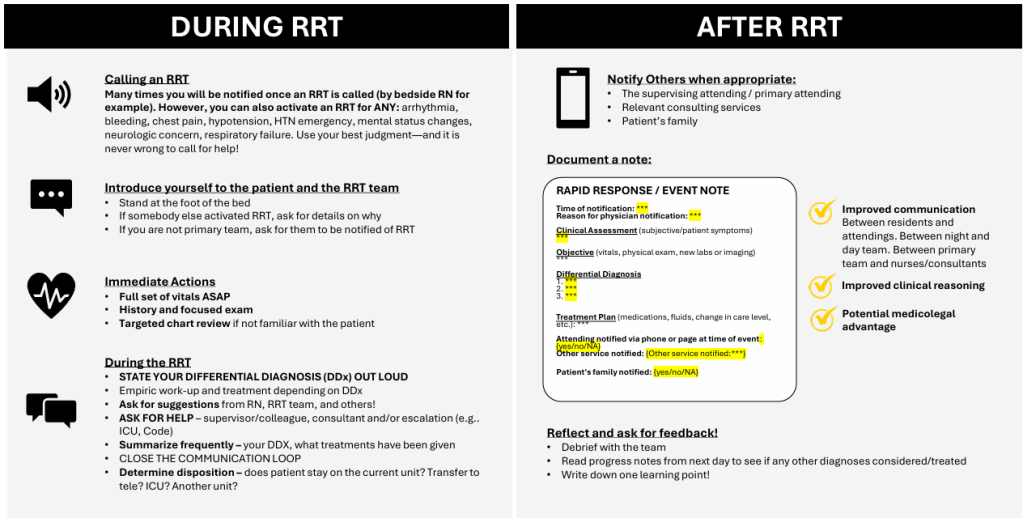
Reviewed and edited by Dr. Jacob Mack, MD
Agitation
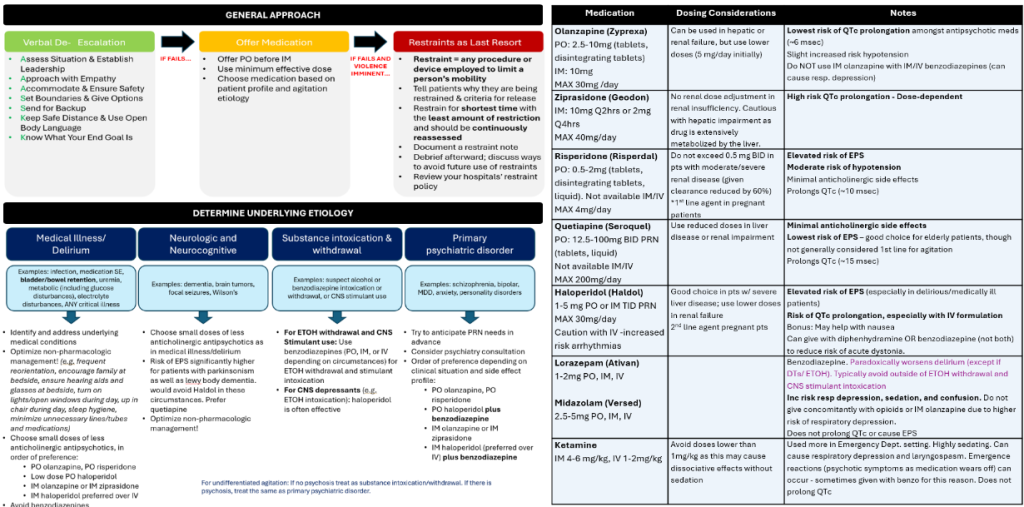
Reference: modified from www.ttreducators.com/compendium
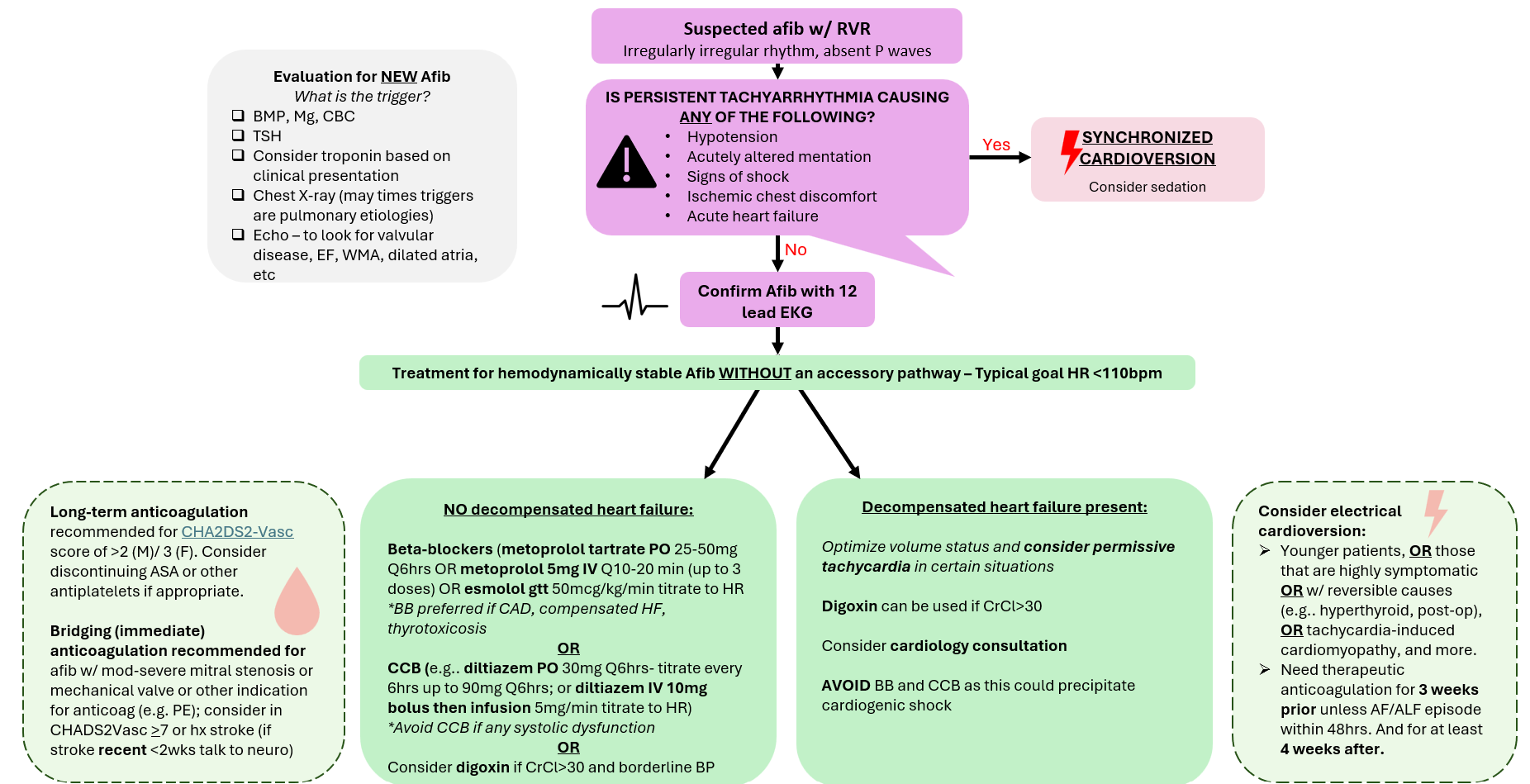
Atrial Fibrillation with RVR
Reviewed and edited by Dr. Marty Tam, MD, MHPE
Altered Mental Status (Acute)

Reviewed and edited by Dr. Kurt Sieloff, MD
Bradycardia with a Pulse

Authors: Dr. Lauren Heidemann MD, MHPE & Dr. Matt Rustici MD
© TTR Course Educators
Reference: 2025 American Heart Association Algorithms
Chest Pain
Reviewed and edited by Dr. Marty Tam, MD, MHPE.
Fever
Reviewed and edited by Dr. Owen Albin, MD.
GI Bleed (Acute)
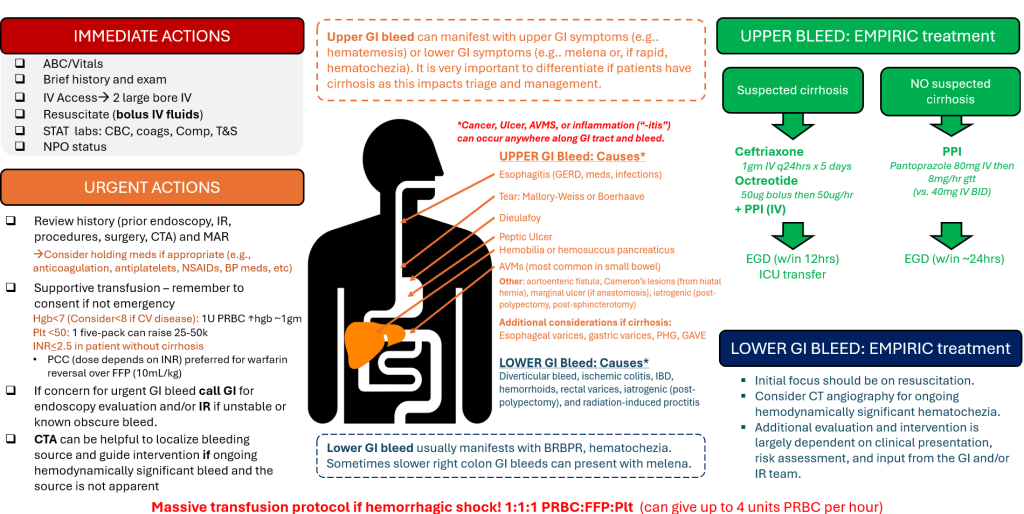
Created by Dr. Amit Gupta, MD, MHPE
Hypertension (Severe)

Reviewed and edited by Dr. Monee Amin, MD
Hypotension
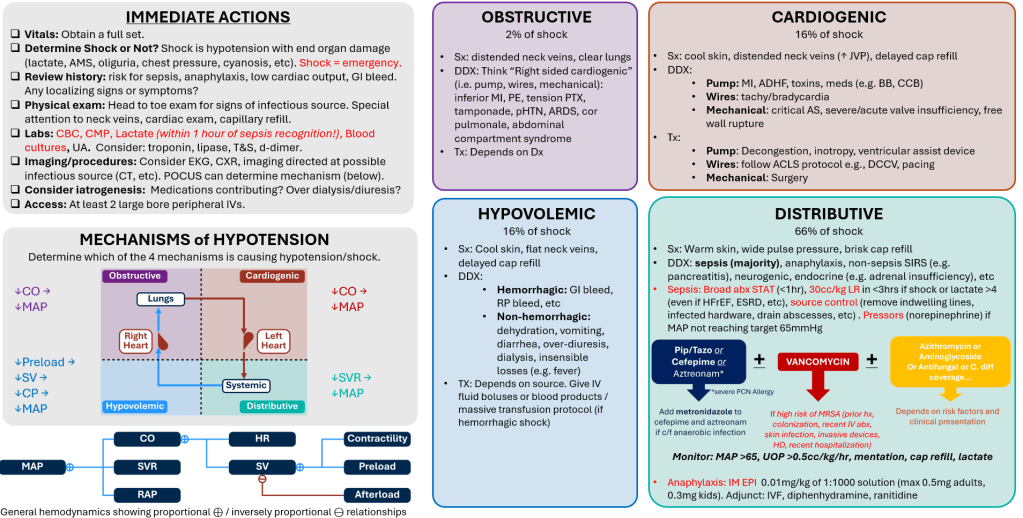
Created by Dr. Jacob Mack, MD
Seizure
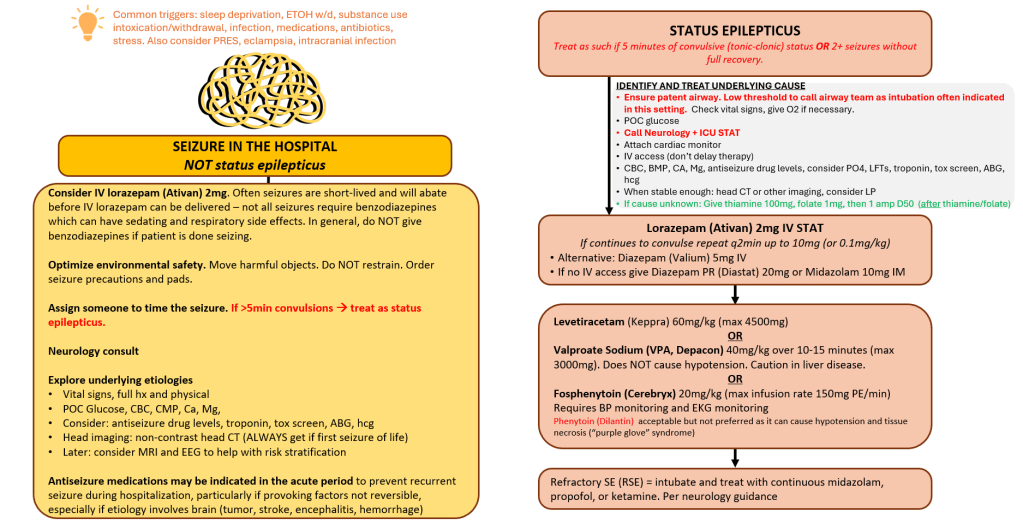
Reviewed and edited by Dr. Kurt Sieloff, MD
Shortness of Breath
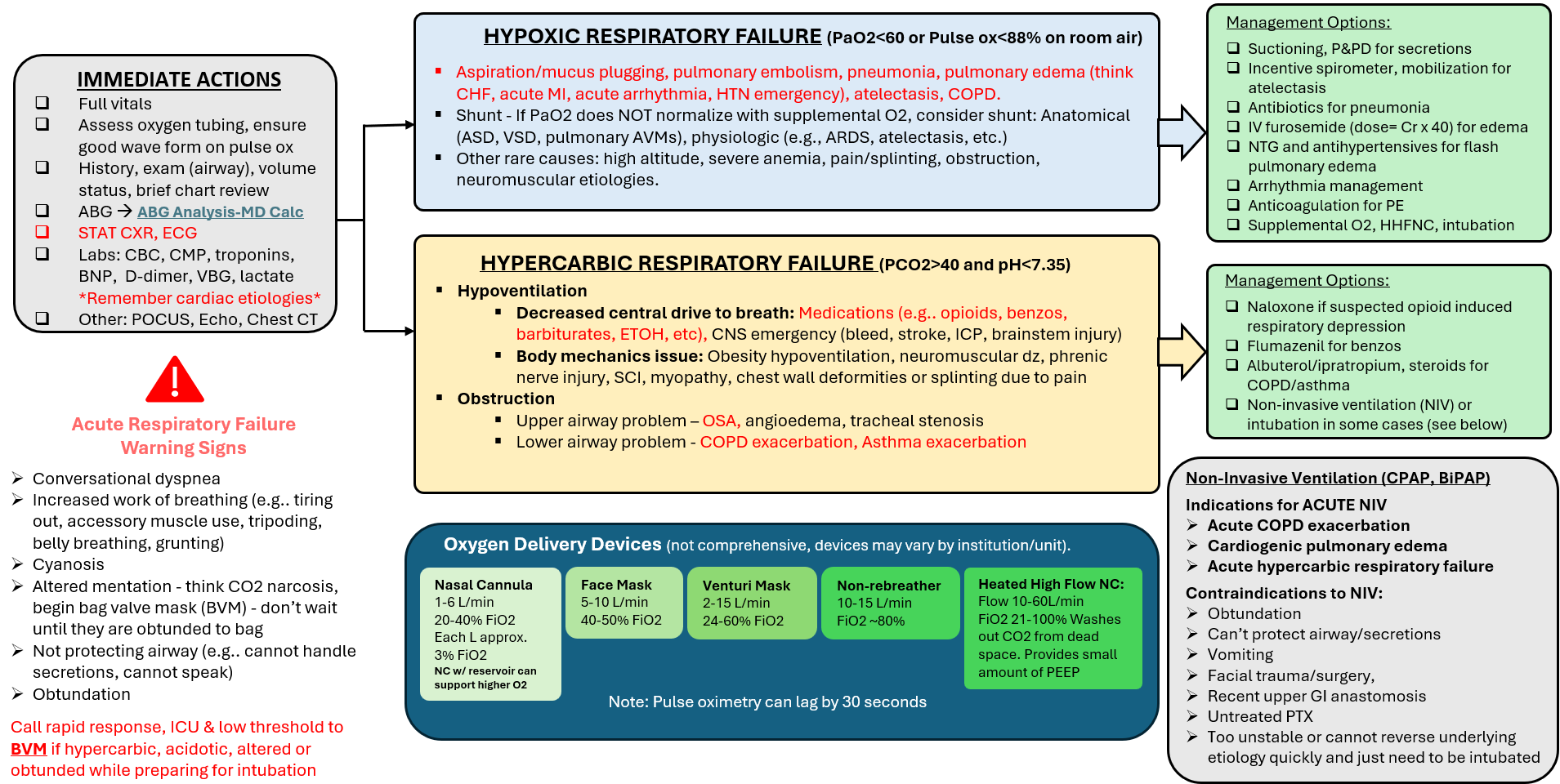
Reviewed and edited by Dr. Kayla Kolbe, MD and Dr. Mark Kolbe, MD
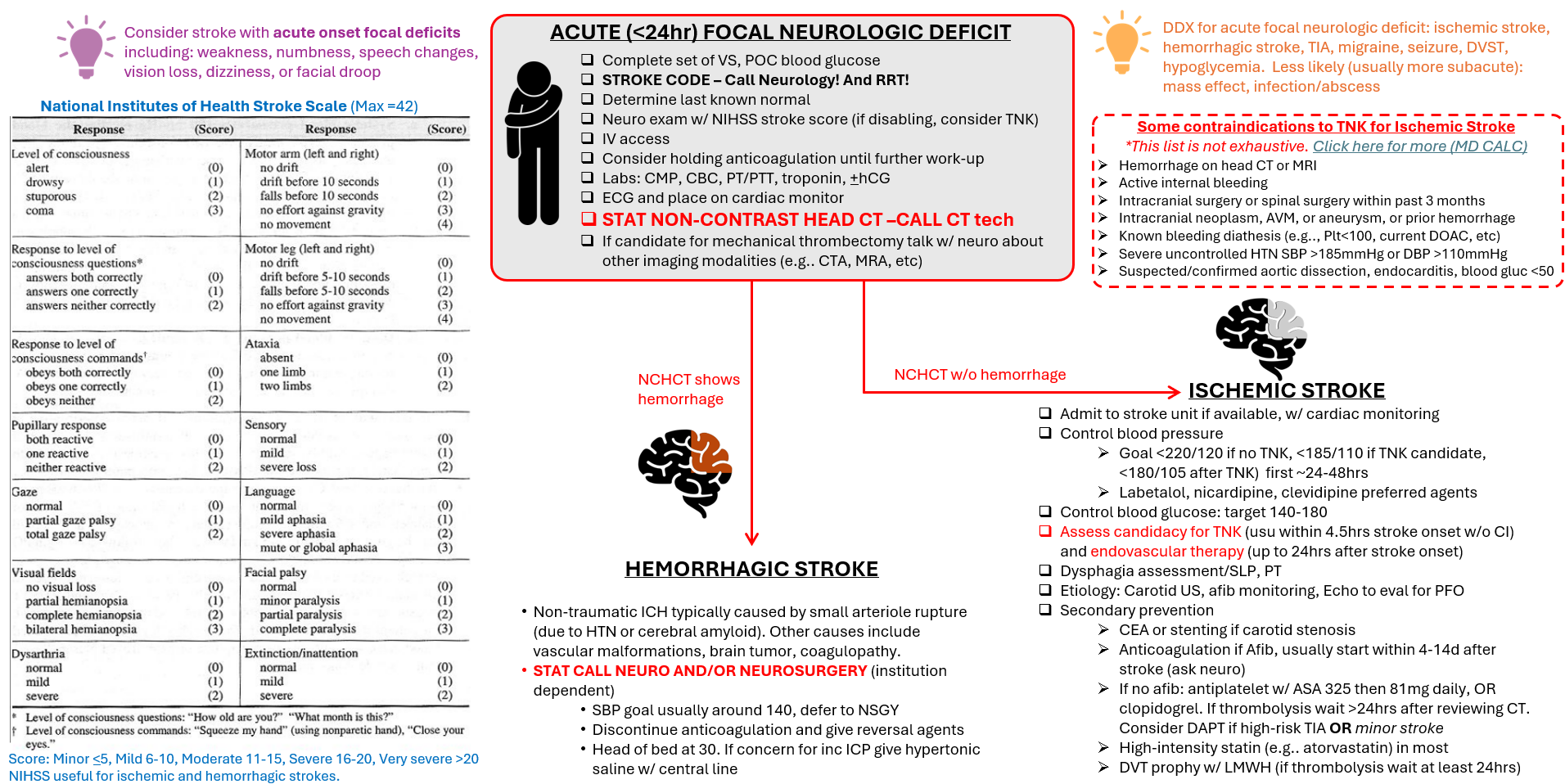
Stroke (Acute)
Reviewed and edited by Dr. Kurt Sieloff, MD
Tachycardia with a Pulse

Authors: Dr. Lauren Heidemann MD, MHPE and Dr. Matt Rustici MD
© TTR Course Educators
Reference: 2025 American Heart Association Algorithm
Common Overnight Cross-Cover Scenarios
GI CONCERNS (Constipation, Diarrhea, Nausea/Vomiting)
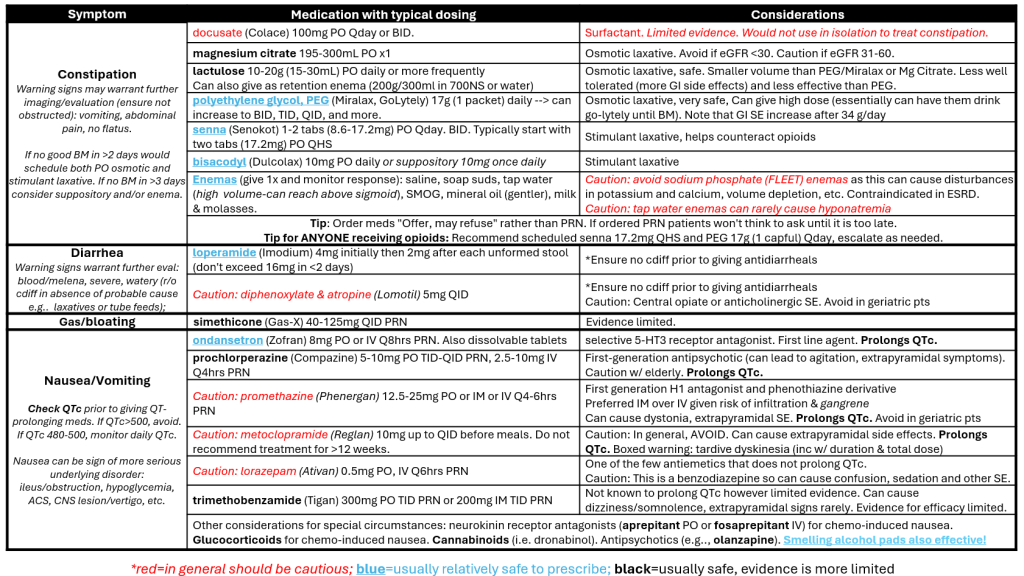
Reviewed and edited by Dr. Jacob, Mack, MD
Insomnia, Cough, Itching, Headache
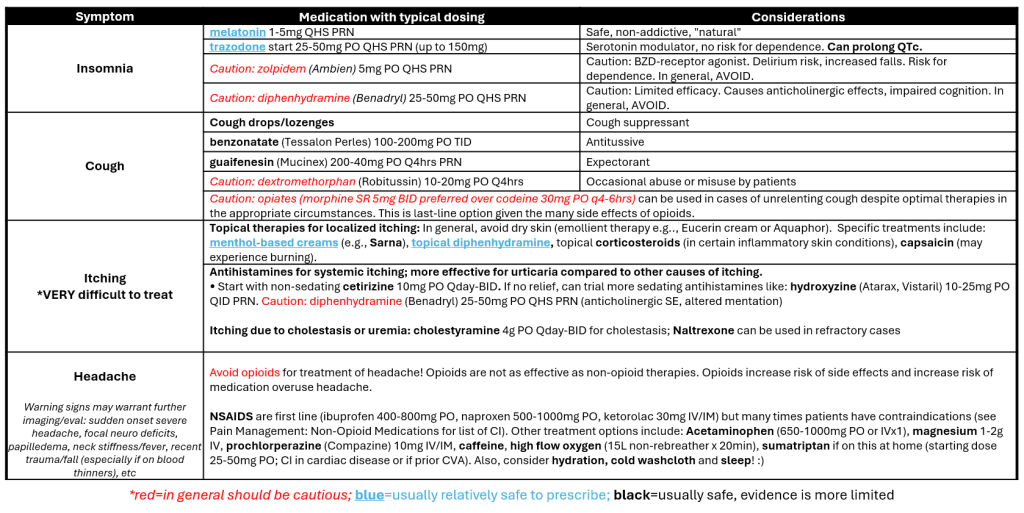
Reviewed and edited by Dr. Kristen E. Fletcher, MD
PAIN MANAGEMENT: Non-Opioid Medications
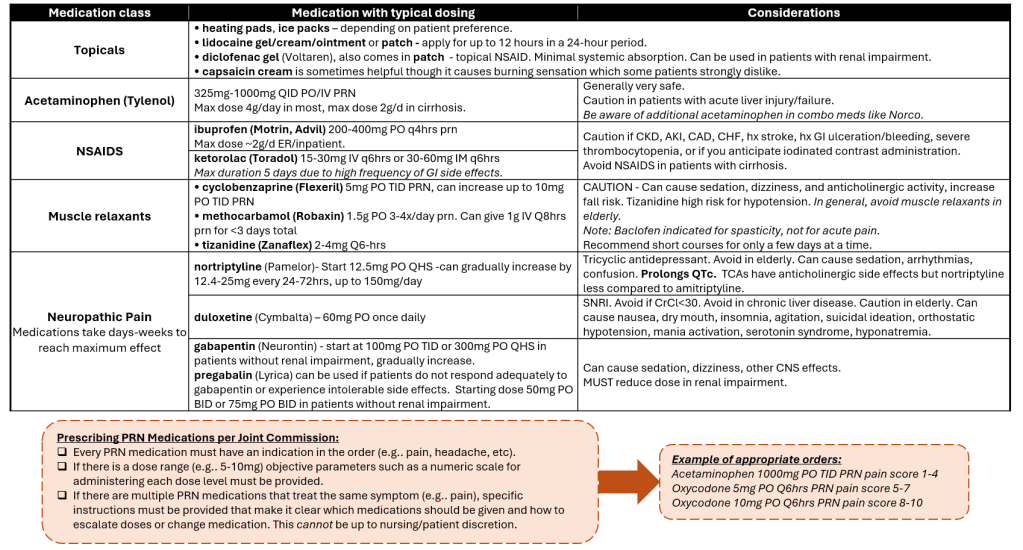
Reviewed and edited by Dr. Kristen E. Fletcher, MD
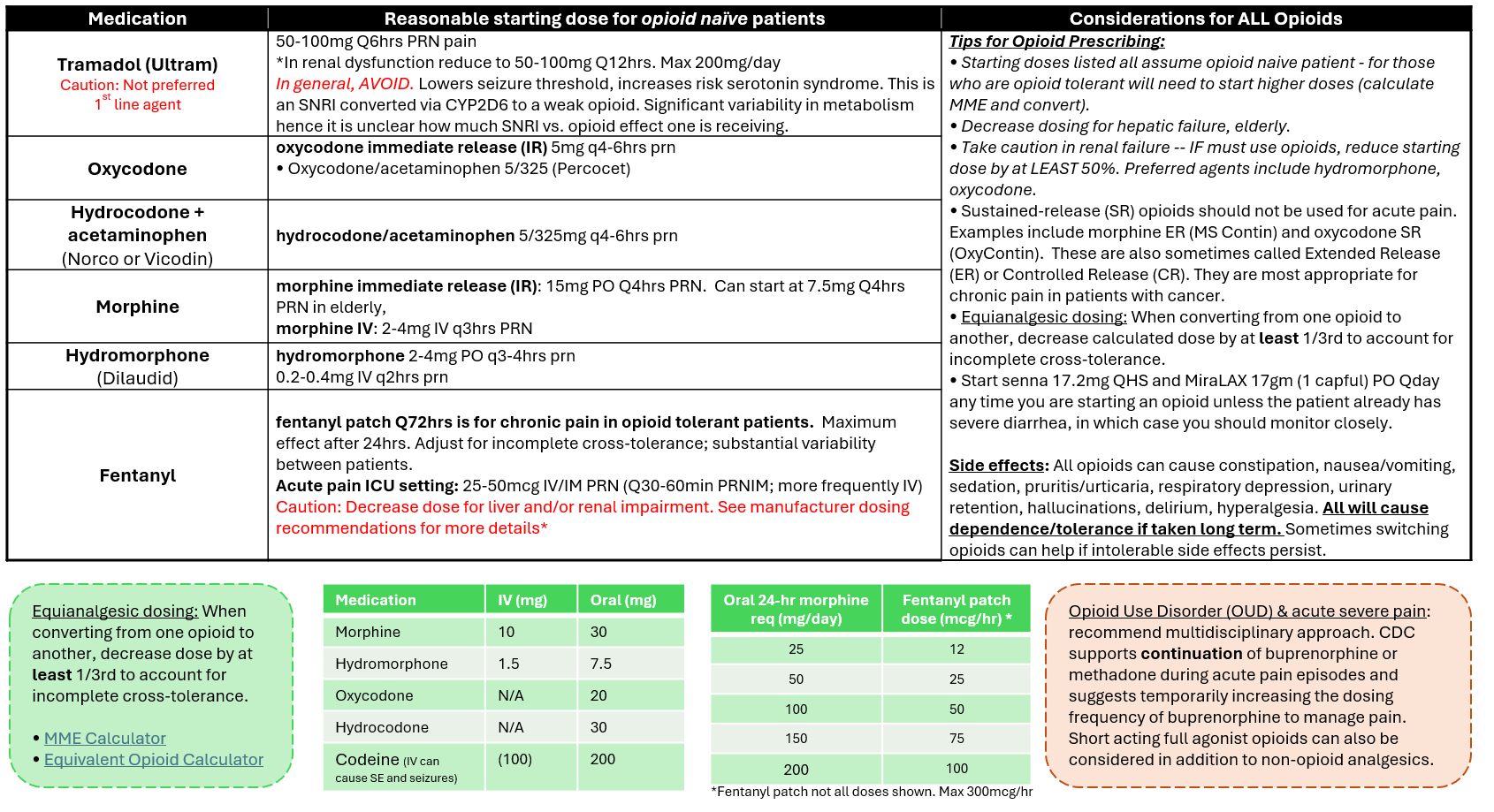
Pain Management: Opioids
Reviewed and edited by Dr. Kristen E. Fletcher, MD
Electrolyte Disorders
SODIUM
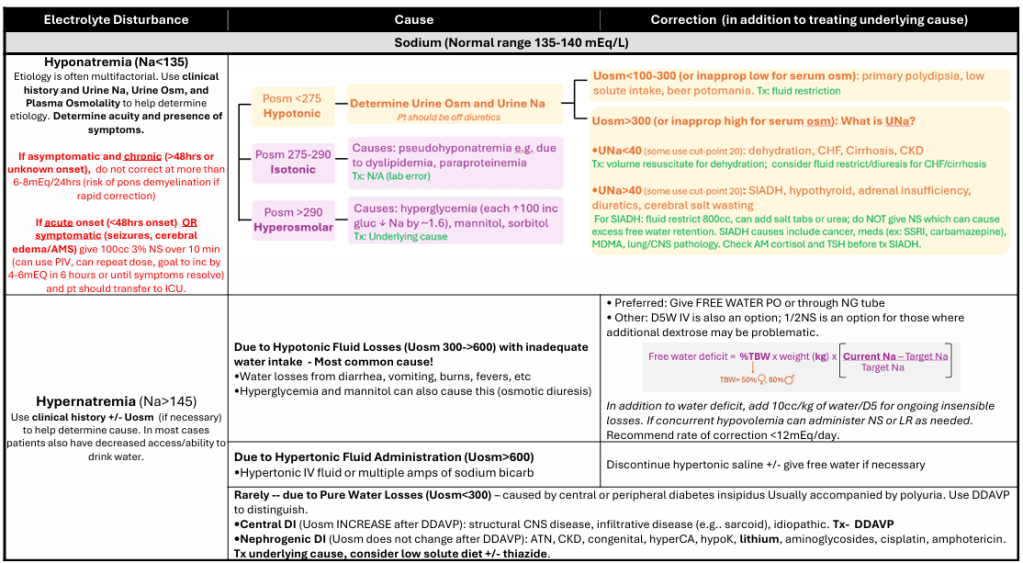
Reviewed and edited by Dr. Junior Uduman, MD, MS, FASN
POTASSIUM AND MAGNESIUM

Reviewed and edited by Dr. Monee Amin, MD
CALCIUM AND PHOSPHORUS

Reviewed and edited by Dr. Junior Uduman, MD, MS, FASN
ABOUT
This guide was created by Dr. Lauren Heidemann, MD, MHPE, a hospitalist at University of Michigan. This project would not have been possible without the expertise, insight, and generous time of many colleagues who reviewed and contributed to the content. Sincere thanks to everyone who helped shape this resource, listed below. This guide is updated annually. Last update January 2026.
- Owen Albin, MD – Infectious Disease specialist at University of Michigan
- Monee Amin, MD- Hospitalist at Emory
- Kristen E. Fletcher, MD – Medicine Pediatrics Hospitalist at University of Kentucky
- Amit Gupta, MD, MHPE – Gastroenterologist at University of North Carolina
- Anna Harleen, MD –Internal Medicine resident at University of California San Francisco
- Kayla Kolbe, MD – Pulmonologist at University of Michigan
- Mark Kolbe, MD – Hospitalist at University of Michigan
- Jacob Mack, MD – Hospitalist at St. Louis VA
- Kurt Sieloff, MD – Neurologist at University of Michigan
- Marty Tam, MD, MHPE – Cardiologist at University of Michigan
- Junior Uduman, MD – Nephrologist at Henry Ford Health
- Julia Witowska, MD – Medicine Pediatrics 4th year Resident at time of review, University of Michigan
(C) Lauren Heidemann. All rights reserved.